

Catheter ablation of atrial tachycardia following atrial fibrillation ablation. Weerasooriya R, Jais P, Wright M, Matsuo KS, et al. Atrial arrhythmias after surgical maze: findings during catheter ablation. Wazni OM, Saliba W, Fahmy T, Lakkireddy D, Thal S, et al. Prevalence, mechanisms, and clinical significance of macroreentrant atrial tachycardia during and following left atrial ablation for atrial fibrillation. 2010 3:243–8.Ĭhugh A, Oral H, Lemola K, Hall B, Cheung P, et al. Circumferential pulmonary vein ablation with additional linear ablation results in an increased incidence of left atrial flutter compared with segmental pulmonary vein isolation as an initial approach to ablation of paroxysmal atrial fibrillation. Atrial tachycardias encountered during and after catheter ablation for atrial fibrillation: part I: classification, incidence, management. Veenhuysen GD, Knecht S, O’Neill Phil D, Wright M, Nault I, Weerasooriya R, et al. Left atrial tachycardia after circumferential pulmonary vein ablation for atrial fibrillation: incidence, electrophysiological characteristic, and results of radiofrequency ablation. 2004 110:1351–7.ĭeisenhofer I, Estner H, Zrenner B, Schreieck J, et al.
Mechanisms of organized left atrial tachycardias occurring after pulmonary vein isolation. Gerstenfeld EP, Callans DJ, Dixit S, Russo AM, Nayak H, Lin D, et al. Late recurrent arrhythmias after ablation of atrial fibrillation: incidence, mechanisms and treatment. Kobza R, Hindricks G, Tanner H, Schirdewahn P, Dorzewski A, et al. Flutter localized to the anterior left atrium after catheter ablation of atrial fibrillation. Jais P, Sanders P, Hsu LF, Hocini M, Sacher F, Takahashi Y, et al. Catheter ablation of long-lasting persistent atrial fibrillation: clinical outcome and mechanisms of subsequent arrhythmias. Haissaguerre M, Hocini M, Sanders P, Sacher P, Sacher F, et al. Catheter ablation for paroxysmal atrial fibrillation: segmental pulmonary vein ostial ablation versus left atrial ablation. Oral H, Scharf C, Chugh A, Hall B, Cheung P, et al. Circumferential radiofrequency ablation of pulmonary vein ostia: a new anatomic approach for curing atrial fibrillation. Papone C, Rosanio S, Oreto G, Tocchi M, Gugliotta F, et al. Electrophysiological end point for catheter ablation of atrial fibrillation initiated from multiple pulmonary venous foci. Haissaguerre M, Jais P, Shah DC, Garrigue S, Takahashi A, Lavergne T, et al. Electrophysiological breakthroughs from the left atrium to the pulmonary veins. Haissaguerre M, Shah DC, Jais P, Hocini M, Yamane T, Deisenhofer I, et al. Spontaneous initiation of atrial fibrillation by ectopic beats originating in the pulmonary veins. Haissaguerre M, Jais P, Shah DC, Takahashi A, Hocini M, Quiniou G, et al.
Catheter ablation flutter series#
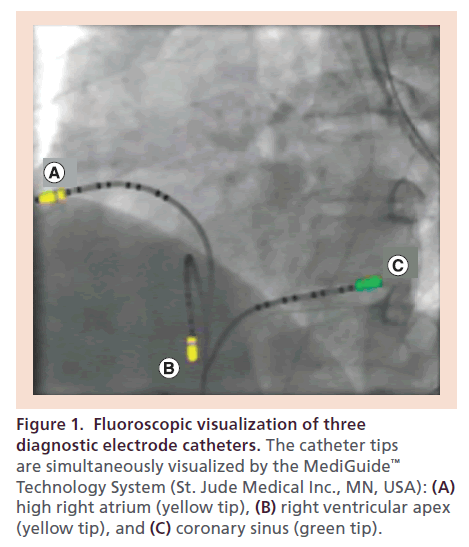
This case series shows that HD-VGM mapping can quickly localize and terminate an atypical flutter circuit. ConclusionsĪblation of atypical atrial flutter is challenging and time consuming. 17.7 ± 7.7 min, p = 0.0021), and success in termination of the arrhythmia during the procedure (100 vs. In comparison to the control cohort, the study cohort had a shorter procedure time (135 ± 46 vs. With a mean follow-up 16 ± 9 months, 90% are in normal rhythm. The mean procedure time was 135 ± 46 min. A mean of 195 ± 75 s of radiofrequency (RF) energy was needed to terminate the arrhythmias. An average 3D anatomic mapping time of 12.39 ± 4.71 min was needed to collect 2996 ± 690 total points and 1016 ± 172 used mapping points. Twenty-six different atypical flutter circuits were evaluated. The results were compared to 21 consecutive historical control patients who had undergone an atypical flutter ablation without HD-VGM. HD-VGM was performed with a commercially available impedance-based mapping system to locate and successfully ablate the critical isthmus of each tachycardia circuit. Twenty-one patients presenting with 26 different atypical atrial flutter circuits after a previous catheter or surgical AF ablation were studied. This study aims to describe a novel method of High Density Activation Sequence Mapping combined with Voltage Gradient Mapping Overlay (HD-VGM) to quickly localize and terminate atypical atrial flutter.


 0 kommentar(er)
0 kommentar(er)
